Pulmonary edema symptoms
Pulmonary Edema: A Comprehensive Guide
Pulmonary edema refers to a medical condition where excess fluid accumulates in the air sacs (alveoli) of the lungs. This buildup interferes with the exchange of oxygen and carbon dioxide, leading to breathing difficulties and reduced oxygen levels in the bloodstream. Pulmonary edema can range from mild to life-threatening and may present as either an acute (sudden) or chronic condition.
Understanding the causes, symptoms, and treatment options for pulmonary edema is essential for effective management and prevention. This guide provides an in-depth look into this condition, helping patients and caregivers navigate its complexities.
What Is Pulmonary Edema?
Pulmonary edema is the abnormal accumulation of fluid in the lungs. Normally, the lungs maintain a delicate balance of moisture to facilitate breathing. In pulmonary edema, this balance is disrupted, resulting in fluid leaking from the small blood vessels (capillaries) into the alveoli. This impairs lung function and leads to symptoms such as shortness of breath, coughing, and chest tightness.
How Does Pulmonary Edema Develop?
The development of pulmonary edema can occur due to heart-related (cardiogenic) or non-heart-related (non-cardiogenic) factors. Cardiogenic pulmonary edema results from increased pressure in the pulmonary veins due to heart dysfunction, whereas non-cardiogenic causes involve direct injury or inflammation of the lung tissues, such as infections or trauma.
Key Types of Pulmonary Edema:
- Acute Pulmonary Edema: Sudden onset of symptoms that requires immediate medical attention.
- Chronic Pulmonary Edema: Develops gradually over time, often as a result of underlying conditions like congestive heart failure.
- High-Altitude Pulmonary Edema (HAPE): Occurs at high altitudes due to reduced oxygen levels.
- Swimming-Induced Pulmonary Edema: Caused by excessive pressure on the lungs during competitive swimming or diving.
Causes of Pulmonary Edema
The causes of pulmonary edema can be categorized into two main types: cardiogenic (heart-related) and non-cardiogenic (not heart-related).
1. Cardiogenic Causes
Cardiogenic pulmonary edema is caused by heart problems that lead to increased pressure in the pulmonary veins. The most common cause is congestive heart failure, where the heart cannot pump blood effectively. This causes blood to back up into the lungs, resulting in fluid leakage. Conditions that may lead to cardiogenic pulmonary edema include:
- Heart attack (myocardial infarction)
- Cardiomyopathy: Weakening of the heart muscle.
- Heart valve disorders: Such as mitral or aortic valve disease.
- High blood pressure (hypertension)
- Arrhythmia: Irregular heart rhythms.
- Myocarditis: Inflammation of the heart muscle.

2. Non-Cardiogenic Causes
Non-cardiogenic pulmonary edema occurs when other factors damage the lungs or cause fluid to leak into the alveoli. These include:
- Acute Respiratory Distress Syndrome (ARDS): Often triggered by severe infections, trauma, or inflammation.
- High-Altitude Pulmonary Edema (HAPE): Resulting from low oxygen levels at high altitudes.
- Pneumonia: A severe lung infection.
- Sepsis: A life-threatening systemic infection.
- Trauma or injury: Direct damage to the lungs.
- Drug overdose: Certain medications or recreational drugs can cause lung damage.
- Pulmonary embolism: A blockage in the pulmonary arteries.
Symptoms of Pulmonary Edema
Acute Pulmonary Edema
Acute pulmonary edema occurs suddenly and is a medical emergency. Symptoms include:
- Severe shortness of breath, especially when lying flat.
- Coughing up frothy, pink-tinged mucus.
- Wheezing or gasping for air.
- Chest pain or tightness.
- Cyanosis (blue-tinged skin or lips) due to low oxygen levels.
Chronic Pulmonary Edema
Chronic pulmonary edema develops gradually, and symptoms may be less severe than in acute cases. These include:
- Persistent shortness of breath, especially during physical activity.
- Swelling in the legs or feet (edema).
- Fatigue and weakness.
- Noisy or wheezing breathing.
Diagnosis of Pulmonary Edema
To diagnose pulmonary edema, healthcare providers will perform a thorough physical examination and may use the following diagnostic tests:
- Chest X-ray: To detect fluid in the lungs.

- Blood tests: To check oxygen levels and identify underlying causes.
- Echocardiogram: To assess heart function.
- Electrocardiogram (ECG): To detect heart rhythm abnormalities.
- CT scan: Provides detailed imaging of the lungs and heart.
Treatment of Pulmonary Edema
The treatment of pulmonary edema depends on the underlying cause and severity of the condition. Options include:
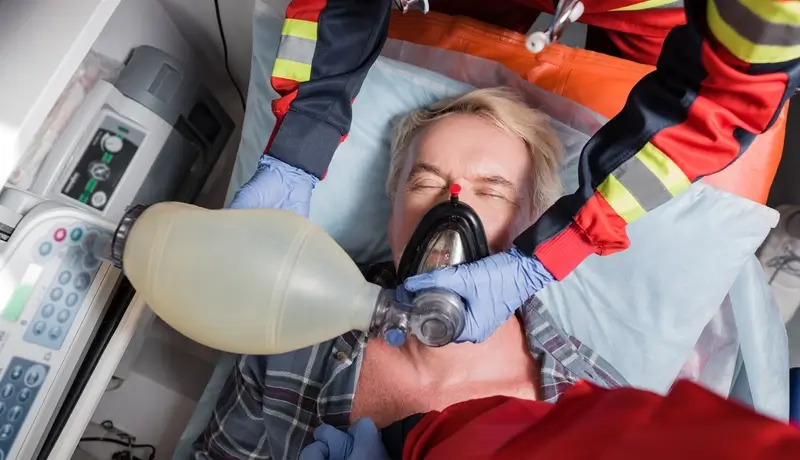
1. Emergency Treatment
- Oxygen therapy to improve oxygen levels.
- Diuretics to remove excess fluid.
- Vasodilators to reduce blood pressure and prevent further fluid accumulation.

2. Long-Term Management
- Treating underlying conditions such as heart failure or kidney disease.
- Lifestyle changes, including a low-sodium diet and regular exercise.
- Medications such as beta-blockers or ACE inhibitors for heart-related causes.
Prevention of Pulmonary Edema
Preventive measures include:
- Managing chronic conditions such as heart disease and diabetes.
- Maintaining a healthy weight and avoiding smoking.
- Staying hydrated and avoiding excessive salt intake.
- Getting regular checkups and vaccinations.
- Avoiding rapid ascents to high altitudes without proper acclimatization.
Conclusion
Pulmonary edema is a serious condition that requires prompt attention. With early diagnosis and appropriate treatment, most patients can recover and lead a healthy life. Understanding the risk factors and symptoms is key to managing and preventing complications. Always consult your healthcare provider if you experience any signs of pulmonary edema.
Frequenlty Asked Questions
-
What lifestyle changes can help prevent pulmonary edema?
Adopting a healthy lifestyle, including maintaining a balanced diet, regular exercise, managing stress, and avoiding smoking, can reduce the risk of conditions like heart disease or high blood pressure that contribute to pulmonary edema. -
Can pulmonary edema occur without any noticeable symptoms initially?
Yes, in some cases, especially chronic pulmonary edema, early symptoms can be mild or unnoticed. Over time, these symptoms may progress to more noticeable signs, such as shortness of breath or fatigue. -
Is pulmonary edema more common in specific age groups or demographics?
Pulmonary edema is more common in older adults, particularly those with pre-existing conditions like heart disease, high blood pressure, or kidney issues. However, it can occur in any age group depending on the underlying cause.
Pulmonary edema symptoms
